In order to grow your bottom line at your independent medical practice, you need to reduce claim denials. Denied claims as well as missing or late charges are two of the most common reasons for lost revenue at an independent medical practice. In order to avoid this, you need to work with a quality RCM services vendor. Together, you and your trusted RCM partner can identify areas that need help and take steps to improve them. Below are 5 steps to reduce claim denials at your independent medical practice.
How Independent Medical Practices Can Reduce Claim Denials
Find the Cause
Finding the cause of why your claims are getting denied is essential. Together, you and your RCM services vendor can identify the root causes for your denied claims. This partnership along with a quality medical billing solution makes it easy to identify areas that need improvement. AI technology automatically notifies providers of red flags in their billing process. Whether the issue is errors in your coding or failure to check eligibility, finding the cause will help you reduce claim denials at your independent medical practice.
Prioritize According to Impact
After identifying the areas that need improvement throughout your billing process, prioritize according to impact. This means moving one step at a time to perfect your revenue cycle and reduce claim denials. If your practice lacks the quality tools it needs to make a change, start your search. Identify a vendor of services that offers what you need and get help to increase clean claims.
Eligibility Verification
Eligibility verification is essential when trying to reduce claim denials at your independent medical practice. Eligibility verification and prior-authorization tools in your software can help you and your patients better prepare. If a patient comes in to receive services and they are not covered, your practice will miss out on a payment. With tools that help you identify and verify coverage prior to a visit, you can reduce claim denials. Once you know a patient is covered, you can gain peace-of-mind that your payment is on the way.
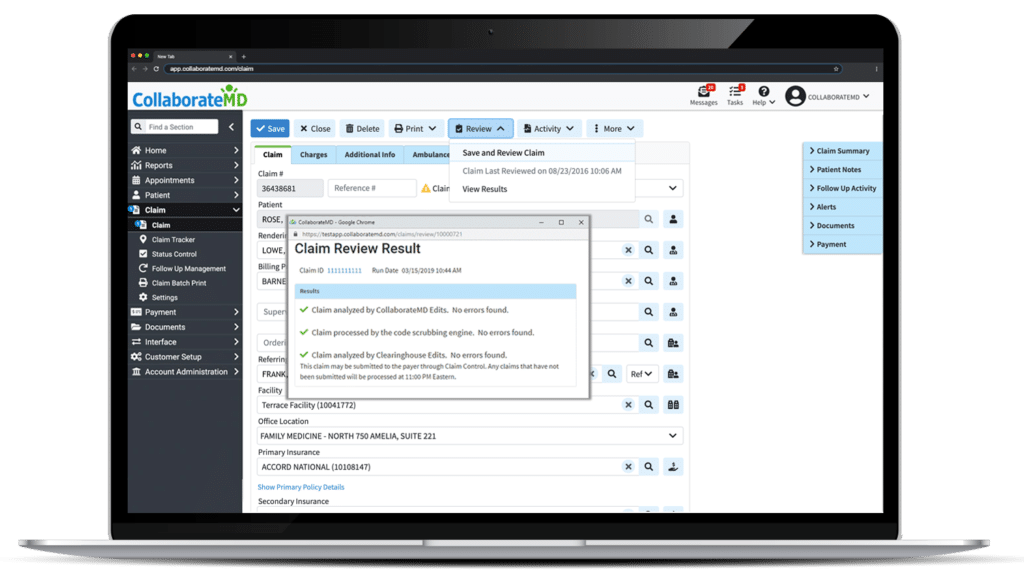
Quality Practice Management Software
Quality practice management software is essential to being able to achieve higher clean claims at your independent medical practice. Without the right technology, your practice won’t be able to get far. Quality medical billing software can give you everything you need to code more effectively, submit charges on time, and identify what parts of your revenue cycle need more attention. The impact of quality technology can not only build your revenue but also streamline your workflow efficiency.
Outsource RCM Services
Lastly, independent medical practices that wish to reduce claim denials need RCM services. Outsourcing RCM services can help your independent medical practice achieve record-high clean claims. They can also reduce the amount of time your accounts spend in A/R by taking over the management of collections and reducing claim denials. Expert billing staff work to ensure your bottom-line climbs above the industry median.
To learn more about quality billing technology or how your practice can partner with a quality RCM services vendor, click here.



